Author:Kangdi 03-11-2023
Being chronically bedridden puts patients at increased risk for painful pressure ulcers and musculoskeletal pain. Finding effective analgesic options that are safe and easy to administer in immobilized patients can be challenging. Topical pain relief patches containing ingredients like lidocaine, diclofenac, and capsaicin are emerging as viable alternatives to oral and injected pain medications for this population.
Several clinical trials have demonstrated the efficacy of specialized prescription lidocaine patches to reduce neuropathic pain, arthritis pain, and pain associated with bone metastases in bedbound individuals. The patches allow for continuous localized delivery of anesthetic to affected areas for up to 12 hours without inducing systemic side effects.
In a study published in the Journal of Pain and Symptom Management, use of lidocaine patches significantly decreased pain scores by an average of 2.3 points on a 10-point scale in hospitalized cancer patients with bone metastases. The patches were well tolerated with minimal skin irritation. This is important, as bed sores are a common issue in immobilized patients.
One trial in the Clinical Journal of Pain also found that lidocaine patches led to a 37% reduction in severe arthritis knee pain in nursing home residents compared to a 22% reduction with diclofenac gel. The lidocaine patch group also reported better physical function. Topical treatments like medicated patches may be preferable to oral NSAIDs in frail seniors who are prone to gastrointestinal bleeding.
Capsaicin patches containing the active compound in chili peppers are another option for prolonged, localized pain relief. Regular use can reduce substance P levels, a neurotransmitter involved in carrying pain signals to the brain. In a study of bedridden patients with neuropathy, capsaicin patches worn for 12 hours significantly reduced pain for up to three months. The patches took effect within four days of use.
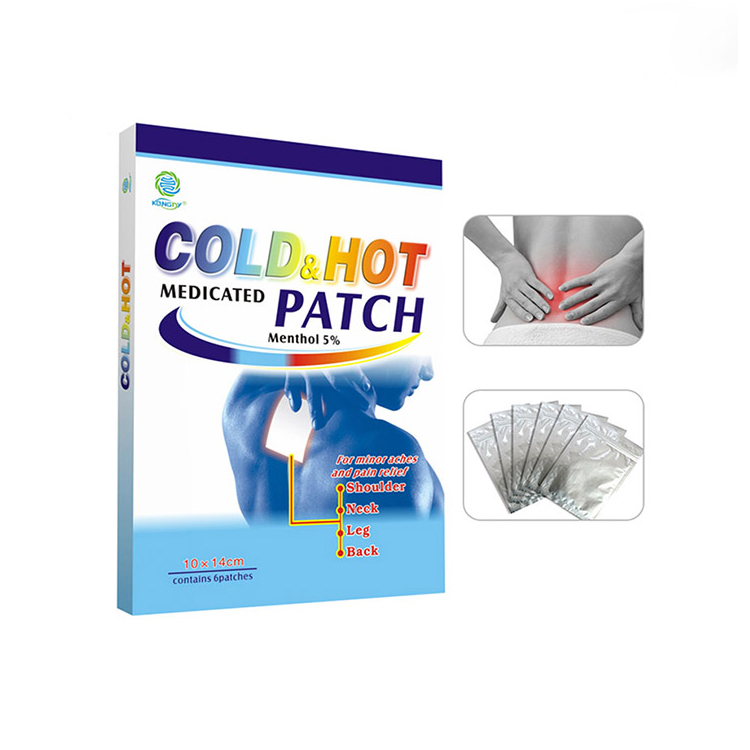
Heating patches that contain menthol, methyl salicylate, and capsaicin may also help relieve muscle soreness and aching joints in immobile patients. The increased circulation from localized warmth can ease stiffness and pain. Combining heating patches with gentle range of motion exercises may provide further benefit, if mobility allows.
To minimize skin irritation, analgesic patches should be applied to clean, dry, intact skin and rotated to different locations daily. Nurses should inspect the area regularly for any redness or rash, especially in patients with fragile skin. Patch ingredients can occasionally trigger allergic reactions or skin breakdown.
Proper patient selection is also important. Lidocaine patches in particular should be avoided in patients with severe liver or kidney dysfunction. Capsaicin may burn or sting initially in some cases. Starting slowly and building up use can improve tolerance.
In conclusion, topical pain relief patches present an attractive analgesic option for chronically bedridden patients who are at risk for medication side effects and skin injuries. Multiple clinical studies support various prescription patch formulations to safely provide localized, sustained pain relief that improves comfort and quality of life in immobilized individuals. With proper precautions and monitoring, pain patches can be an effective element of a comprehensive pain management regimen for bedbound patients.
 0086 19937104978
0086 19937104978